Prostate Cancer: Causes, Symptoms, Testing, Risk Factors & Treatment
Prostate cancer is the most common cancer among men in many countries — including Sweden, the UK, and the United States. While it often grows slowly and without symptoms, aggressive forms can spread rapidly and become life-threatening if not caught early.
This comprehensive guide covers everything you need to know about prostate cancer: what it is, how it develops, early warning signs, risk factors, modern detection methods like the Stockholm3 test, and available treatment options.
Contents
What Is Prostate Cancer?
Who Gets Prostate Cancer?
Symptoms of Prostate Cancer
Risk Factors
How Prostate Cancer Is Detected
The Stockholm3 Test
Diagnosis & Staging
Treatment Options
Living with and After Prostate Cancer
Prevention and Lifestyle Tips
Frequently Asked Questions
1. What Is Prostate Cancer?
The prostate is a small, walnut-sized gland located just below the bladder in men. It surrounds the urethra (the tube that carries urine out of the body) and plays an important role in semen production.
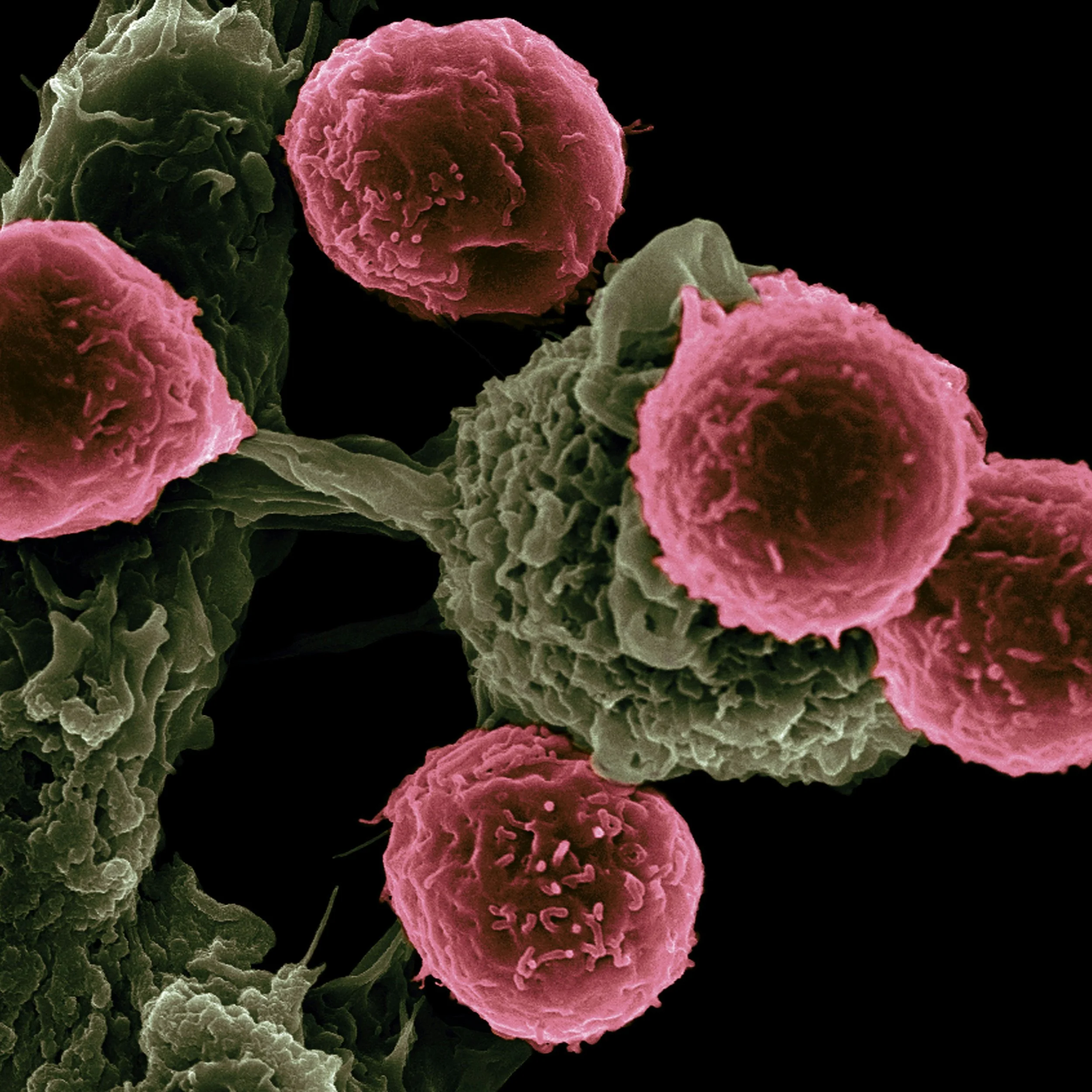
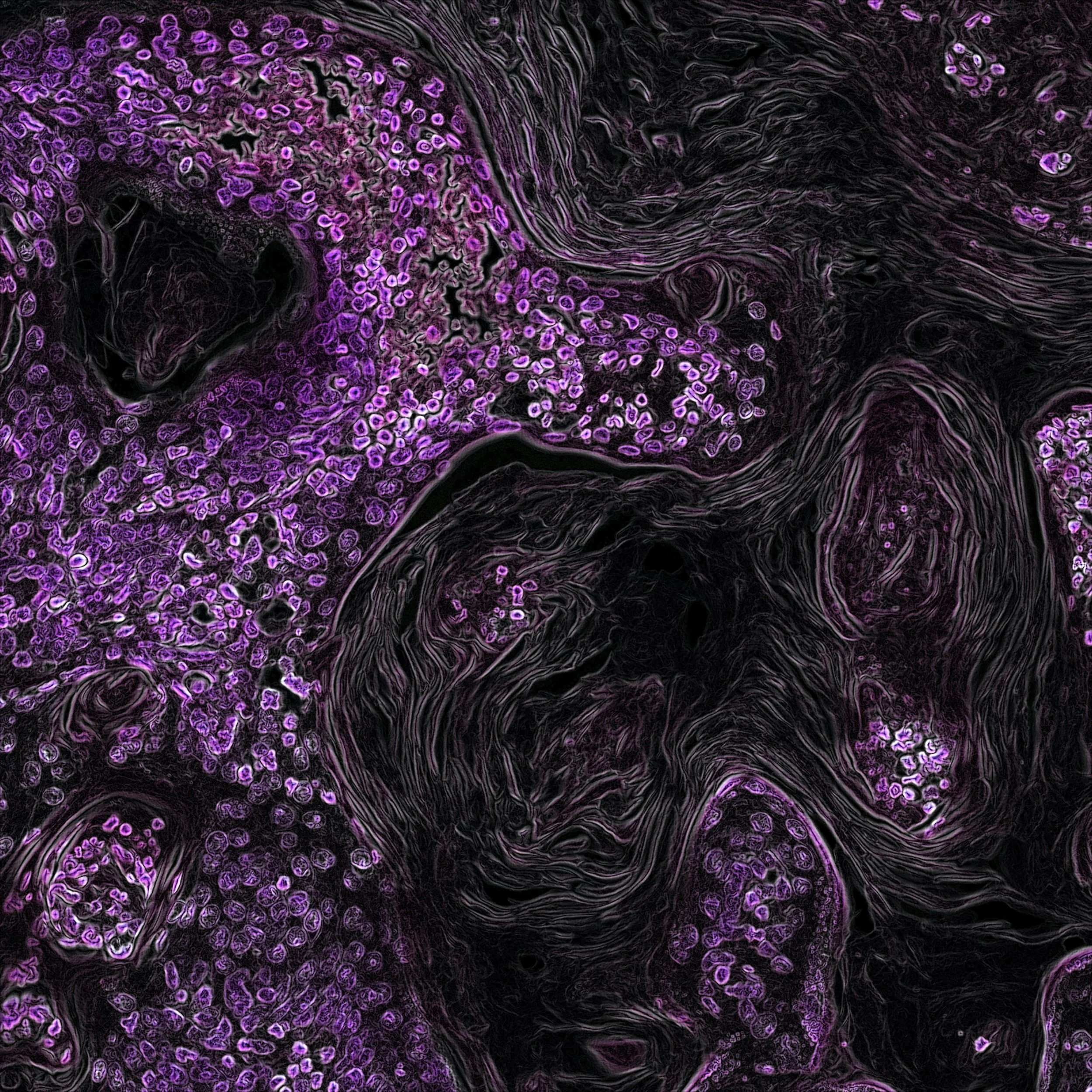
Prostate cancer occurs when cells in the prostate gland begin to grow uncontrollably, forming a tumor. In many cases, these tumors are slow-growing and may never cause harm. But some forms are aggressive and can spread to other parts of the body, particularly the bones and lymph nodes.
2. Who Gets Prostate Cancer?
It's estimated that 1 in 8 men will be diagnosed with prostate cancer during their lifetime.
In Sweden alone, over 10,000 new cases are diagnosed each year.
It’s most common in men over 50, and especially those over 65.
While some men live for decades with low-risk prostate cancer, others develop life-threatening forms that require prompt and aggressive treatment.
3. Symptoms of Prostate Cancer
In its early stages, prostate cancer often causes no symptoms at all. When symptoms do appear, they may include:
Difficulty starting or stopping urination
Weak or interrupted urine stream
Frequent urination, especially at night
Pain or burning sensation when urinating
Blood in urine or semen
Erectile dysfunction
Pain in the lower back, hips, or pelvis (suggests advanced disease)
Important: These symptoms can also result from benign prostate enlargement (BPH), but they should always be evaluated by a healthcare professional.
👉 Learn more: [Full article on symptoms of prostate cancer]
4. Risk Factors
Several factors can increase your likelihood of developing prostate cancer:
Non-modifiable factors
Age: Risk rises sharply after age 50.
Family history: If your father or brother had prostate cancer, your risk doubles.
Genetics: BRCA1, BRCA2, and other inherited gene mutations increase risk.
Ethnicity: Men of African descent are at higher risk.
Modifiable factors
Diet: High-fat, low-vegetable diets may increase risk.
Obesity: Linked to more aggressive cancer.
Smoking and heavy alcohol use: Associated with worse outcomes.
Sedentary lifestyle: Increases risk and lowers overall health.
👉 Learn more: [Risk factors and prevention]
5. How Prostate Cancer Is Detected
The most common ways to detect prostate cancer include:
➤ PSA Test
Measures prostate-specific antigen levels in the blood. High levels may suggest cancer, but false positives are common.
➤ Digital Rectal Exam (DRE)
A physical examination where a doctor feels the prostate through the rectal wall to detect abnormalities.
➤ Stockholm3 Test
A more advanced blood test that combines biomarkers, genetics, and clinical data to provide a highly accurate risk assessment.
➤ MRI and Biopsy
If blood tests show high risk, an MRI and tissue biopsy are performed to confirm diagnosis and determine cancer grade.
👉 Learn more: [How prostate cancer is detected]
6. The Stockholm3 Test
The Stockholm3 test is a next-generation blood test developed in Sweden to detect aggressive prostate cancer more accurately than PSA.
It includes:
PSA + 4 additional protein markers
Over 100 genetic risk variants
Age, family history, and other clinical factors
Benefits:
Reduces unnecessary biopsies by up to 50%
Detects 30% more aggressive cancers
Provides a personalized risk score (0–100%)
It is increasingly used in clinical practice across Sweden, Norway, and parts of Europe.
👉 Learn more: [Stockholm3 test explained]
7. Diagnosis and Staging
If cancer is confirmed via biopsy, it is graded and staged to determine severity and treatment options.
➤ Gleason Score
Assesses how abnormal the cancer cells look under a microscope:
6 = Low-grade cancer
7 = Intermediate
8–10 = High-grade and more aggressive
➤ Staging (TNM system)
T: Size and extent of tumor in prostate
N: Has it spread to lymph nodes?
M: Has it metastasized to other organs?
Imaging tests (MRI, bone scans, CT) may be used to assess spread.
8. Treatment Options
Treatment depends on the stage and aggressiveness of the cancer, as well as your age and overall health.
➤ Active Surveillance
For low-risk cancers. Includes regular PSA tests, MRIs, and occasional biopsies. No immediate treatment needed.
➤ Surgery (Prostatectomy)
Removal of the prostate gland. May cause side effects like urinary incontinence or erectile dysfunction.
➤ Radiation Therapy
Can be delivered externally or via internal seed implants (brachytherapy).
➤ Hormone Therapy
Reduces androgen levels (testosterone), which fuel cancer growth.
➤ Chemotherapy & Immunotherapy
Used in advanced or hormone-resistant cancer.
👉 Learn more: [Guide to prostate cancer treatment options]
9. Living with and After Prostate Cancer
Prostate cancer affects more than just physical health — it can impact your:
Urinary function
Sexual health
Mental well-being
Relationships and quality of life
Tips for navigating survivorship:
Don’t be afraid to ask for psychological support
Explore pelvic floor therapy for incontinence
Seek sexual health counseling if needed
Join support groups to connect with others
Thanks to early detection and modern treatments, millions of men live full lives after a prostate cancer diagnosis.
10. Can Prostate Cancer Be Prevented?
There’s no guaranteed way to prevent prostate cancer, but research suggests you can reduce your risk by:
✅ Eating more fruits, vegetables, and fiber
✅ Limiting red meat and dairy fats
✅ Exercising regularly
✅ Maintaining a healthy weight
✅ Avoiding tobacco and excess alcohol
✅ Considering testing if you’re over 50 — or 45 with risk factors
👉 Learn more: [Prostate cancer prevention and diet]
11. Frequently Asked Questions
Q: Is prostate cancer always serious?
A: No. Many prostate cancers grow slowly and never cause harm. But aggressive forms can spread and become life-threatening if not treated.
Q: What age should I start testing?
A: Generally, men should consider testing around age 50 — or 45 if they have a family history or are at higher risk.
Q: Is PSA a reliable test?
A: It can help detect issues, but it's not specific. False positives are common. That’s why more advanced tests like Stockholm3 are gaining ground.
Q: Will treatment affect my sex life?
A: Some treatments can cause erectile dysfunction, but many men recover with time, therapy, or medication.
Final Thoughts
Prostate cancer is a complex disease — sometimes silent and slow, other times aggressive and fast-moving. The good news is that with modern diagnostics and personalized care, more men than ever are surviving and thriving after diagnosis.
Whether you’re over 50, have a family history, or simply want to take control of your health, learning about your individual risk and testing options — like the Stockholm3 test — is a smart and proactive step.
📚 Continue Reading:
[Symptoms of Prostate Cancer – What to Watch For]
[How the Stockholm3 Test Works]
[Best Diet and Lifestyle Tips to Reduce Risk]